Oral Health and Scleroderma

Every human being should enjoy oral health that is good enough to allow them to eat, drink or speak every day of their life. However, scleroderma often interferes with these essential actions, either directly by disrupting the physiological function of the oral space, or indirectly by significantly hindering hygiene methods. Fortunately, most people living with scleroderma will not experience the full range of these problems, and the severity of symptoms will vary from person to person.
This text is not intended to be scientific or exhaustive. Its goal is to address the main known concepts to better understand how a disease like scleroderma can affect the function of this unique part of the body: the mouth.
Let us explore how scleroderma influences oral health and the various approaches that can help improve quality of life for many people who may face these challenges.
And let us also emphasize the importance of consulting a dental professional regularly as soon as the first symptoms of scleroderma appear, in order to prevent or limit the progression of oral complications described below.
 |
MICROSTOMIA The skin of the face loses elasticity, and mouth opening can become significantly restricted. This leads to difficulties with speaking and eating, especially as the tongue may lose mobility and the lingual frenulum, a thin membrane connecting the tongue to the floor of the mouth, may become fibrotic and limit movement. Basic hygiene routines become harder to carry out, and dental visits may be uncomfortable or even impossible to perform properly, particularly in the back areas of the mouth. Facial skin thickening may also cause the teeth to shift due to the pressure applied to them. It can also worsen dryness in the mouth because of an inability to close the lips and achieve a proper seal, leaving the mouth slightly open at all times. Clearly informing your dentist about your scleroderma diagnosis allows care to be properly adapted to your needs, whether it involves the duration of the procedures, a more comfortable position, the choice of instruments, or the type of restoration if needed, to make treatment easier and more comfortable. |
STRATEGIES FOR IMPROVEMENT
Numerous studies show that positive results can be achieved through daily stretching exercises of the mouth using fingers or tongue depressors. These exercises need to be performed several times a day to yield meaningful improvements. Physical therapy, kinesiology and occupational therapy can also offer relevant exercises and techniques. In more severe cases, hyaluronidase injections may be used to soften the skin, along with autologous fat grafts taken from the patient, or IPL treatment, a technique using intense pulsed light.
Toothbrushes with small heads or designed for children, or electric toothbrushes with rotating heads and larger handles, can help improve access to back teeth. Interdental brushes and oral irrigators, such as Waterpik, may also be considered. If subtle dental shifting causes discomfort when chewing or muscle pain, the dentist can perform minor adjustments by carefully grinding the teeth that no longer fit together properly. More frequent dental visits, ideally every three months, are highly recommended to detect and prevent issues before they arise and require longer or more demanding treatments. In addition, when cleanings are done more often, they are much quicker.
For more details, see: “Dermatological Interventions for Facial Manifestations of Scleroderma”.
XEROSTOMIA
Dry mouth caused by reduced saliva flow
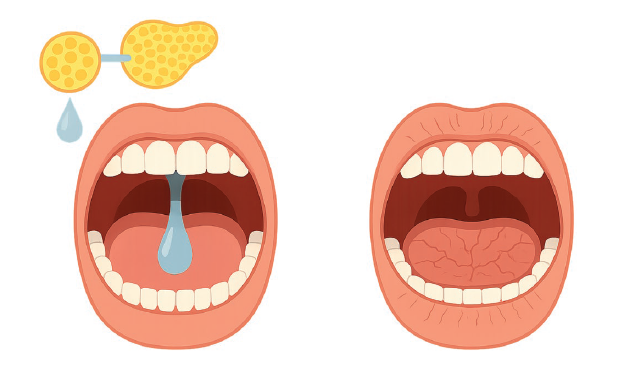 |
Many people with scleroderma experience xerostomia. Fibrosis can affect the salivary glands, but in some cases, it is Sjögren’s syndrome, a chronic, systemic autoimmune condition, that is responsible. Both lead to similar effects: an irreversible reduction in saliva flow, resulting in a dry mouth. Saliva lubricates the mouth, helping with speech and swallowing. It cleans food debris and contains substances that neutralize the acid produced by oral bacteria and that help remineralize tooth enamel. It also contains components that help control the number of microbes and viruses in the mouth. Reduced saliva flow clearly increases the risk of tooth decay and enamel erosion, mainly due to the heightened acidity in the mouth. Dryness also affects the comfort and fit of removable prostheses. Xerostomia can also disturb the oral microbial balance, leading to candidiasis, fungal infections caused by microscopic yeast, especially under prostheses or in the corners of the lips, where they trigger painful inflammation known as angular cheilitis.
|
STRATEGIES FOR IMPROVEMENT
|
To help compensate for reduced saliva flow, it is recommended to:
Saliva substitutes, lubricants, and saliva stimulants are available over the counter, such as lozenges, or by prescription, such as pilocarpine. |
To reduce the risk of cavities, it is advised to:
In case of candidiasis, dentists can prescribe antifungal creams, which are usually effective. For more persistent cases, oral medication may be used.
|
For more information, see: “Sjögren’s Syndrome Associated with Systemic Scleroderma”.
TOOTH DECAY
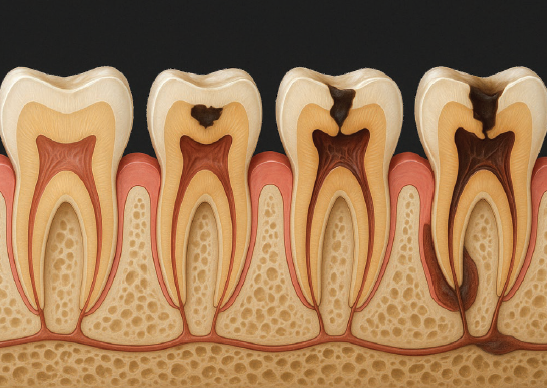 |
Tooth decay is the most widespread infectious disease in the world. According to the World Health Organization, nearly all adults have had cavities. It is rare to find someone who has never had one. People living with scleroderma who also experience microstomia, xerostomia, gastroesophageal reflux, or reduced manual dexterity are especially at risk. When the mouth opening is limited and hand movements are difficult, brushing and flossing become extremely challenging. Xerostomia is an aggravating factor for the development of new tooth decay because it reduces the beneficial effects of saliva. Saliva normally helps clear food particles from teeth, neutralizes acid, and strengthens enamel. Gastroesophageal reflux, or GERD, increases the presence of acid in the mouth. This further raises the risk of cavities and contributes to enamel erosion. |
STRATEGIES FOR IMPROVEMENT
Dental plaque must be removed regularly. It contains salivary proteins, food debris, and many bacteria that turn sugars into acid. This includes natural sugars such as those found in honey, maple syrup, or fruit. The acid then attacks the enamel, eventually creating a cavity, and can also irritate the gums. Reducing sugar intake, whether from foods or drinks, helps protect teeth. Bacteria make no distinction. They use all forms of sugar to produce acid.
People who are at higher risk of cavities or who experience frequent tooth decay would certainly benefit from fluoride. This natural element strengthens enamel and helps reduce the number of bacteria that produce acid. Its antimicrobial and protective action makes the enamel more resistant to acid attacks. Fluoride is available in many forms. It is helpful to speak with your dental team to choose the best options for your situation.
There are high-fluoride toothpastes available, such as Colgate PreviDent Booster Plus, which contains 5000 ppm fluoride and is safe for regular use. Fluoride gels applied at night using trays may also be recommended. Topical creams containing calcium, phosphate, and fluoride, such as MI Paste Plus, can be useful for people with low saliva flow. Fluoride varnish applied professionally at the dental office, as is done with children, is also well suited for adults at high risk of cavities. In addition, the occlusal or chewing surface of molars can be sealed to block bacteria from settling in grooves and to make cleaning easier.
Daily exercises to maintain or increase mouth opening and hand mobility are valuable. They make oral hygiene easier to perform at home. These exercises are described in the educational sheet “The Scleroderma Patient-centered Intervention Network (SPIN) and the SPIN-HAND Program.”
Toothbrushes with adapted handles or electric toothbrushes can improve grip for those with limited dexterity. Floss holders and interdental brushes are also practical tools to replace regular flossing when needed.
PERIODONTAL DISEASE
Gingivitis and periodontitis worsened by scleroderma
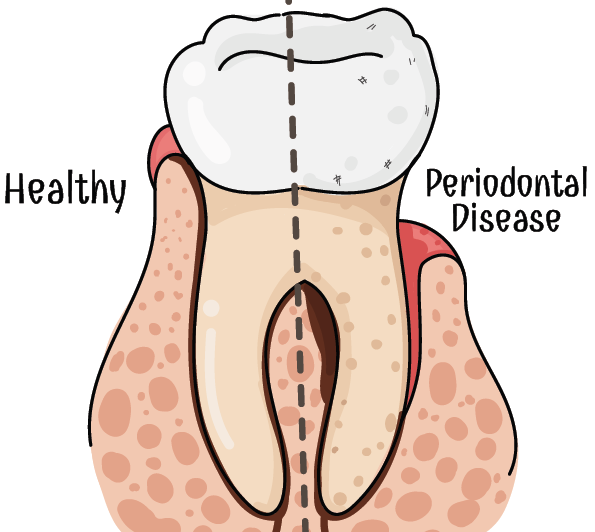 |
The periodontium refers to the set of tissues that support the teeth, namely the bone, the periodontal ligament, and the gum. The root is firmly anchored in the jawbone, covered with a protective layer called cementum, and held in place by small fibers that form the periodontal ligament. The gum acts as a protective tissue over the bone. Many adults suffer from periodontal disease, which often leads to tooth loss due to the gradual destruction of these supporting tissues by bacteria. A tooth may appear completely normal, with no decay or visible wear, but without a solid anchor in the bone, its stability and long-term survival are compromised. Scleroderma can increase the severity of periodontal disease through fibrosis of the oral mucosa and frena, creating tension on the gums and thereby increasing gingival recession, that is, receding gums. In addition, microstomia and reduced manual dexterity greatly complicate the hygiene techniques essential for eliminating the bacteria responsible for gum inflammation, known as gingivitis, as well as the possible damage to the supporting structures of the teeth, known as periodontitis. Furthermore, reduced saliva flow worsens the situation, since its cleansing and bacterial-regulating roles are compromised.
|
STRATEGIES FOR IMPROVEMENT
The simplest and most effective way to prevent periodontal disease is to remove dental plaque loaded with bacteria before they produce enough toxins and acid to first damage the gums, then reach deeper areas and cause bone resorption, meaning a progressive loss of the bone that supports the teeth.
Therefore, with each brushing, it is important to pay close attention to the gumline by gently massaging this area using a soft-bristled toothbrush. The same applies to dental floss, which should be adapted to the curved surface of the tooth to dislodge bacteria hidden beneath the gum. Floss can be gently inserted under the gum without risk.
Your dental hygienist is without a doubt the best person to teach you these techniques. Your hygienist or your dentist is also the one who can effectively remove tartar deposits, which are made up of hardened or calcified dental plaque, using specialized instruments, as this cannot be done with a toothbrush. Tartar also harbors a large number of bacteria that can cause irreversible damage to the periodontium. It is therefore essential to remove these deposits regularly to avoid progressive deterioration that could lead to tooth loss.
GASTROESOPHAGEAL REFLUX DISEASE (GERD)
Oral acidity and tooth enamel erosion
 |
GERD, which is common among adults, is even more frequent in people living with scleroderma. The esophagus, the tube that connects the mouth to the stomach, may have weak or ineffective contractions, and the lower esophageal sphincter, which is the valve that separates the esophagus from the stomach, may become deficient and fail to close properly. This results in the backflow of stomach acid and bile into the esophagus, sometimes reaching the mouth. The acid produced by the stomach has a very low pH, between 1 and 3, whereas a neutral pH, like that of most drinking water, is 7. This extreme level of acidity makes it particularly aggressive or damaging to tooth enamel. When saliva production is also reduced, a condition known as hyposialia, this acidity becomes even more harmful. Unfortunately, lost enamel does not regenerate naturally. Once it is damaged, it can only be restored through dental treatments.
|
STRATEGIES FOR IMPROVEMENT
There are several proven techniques to help reduce GERD:
-
Keep the head of the bed raised to prevent acid from rising during sleep.
-
Avoid eating during the three hours before going to bed.
-
Limit or avoid caffeine, alcohol, fatty foods, chocolate, and acidic drinks.
-
Drink water regularly or rinse the mouth frequently.
-
Avoid sugary foods and drinks, since oral bacteria turn them into acid.
For more information, see: “The Digestive System and Systemic Scleroderma.“
In more serious cases, antacids or medications such as proton pump inhibitors may be prescribed to reduce stomach acid production. It is also recommended to use fluoride in all its forms. This includes toothpaste, fluoride varnish, gels, and topical creams. Fluoride helps protect enamel by making it more resistant to acid and supporting remineralization.
The amount of enamel already lost cannot be naturally restored. Severely eroded areas may eventually require dental restorations, such as fillings, crowns, or inlays. However, if the remaining enamel becomes stronger and more resistant to acid, further damage can be significantly reduced.
TMJ AND FACIAL PAIN
Temporomandibular Joint and muscle or nerve pain
 |
The temporomandibular joint, or TMJ, connects the lower jaw to the skull. It is located on each side of the face, just in front of the ears. This joint is complex and allows a wide range of motion, which often makes it prone to discomfort. Scleroderma can affect this joint just as it affects other joints in the body. Muscle fibrosis, reduced blood flow, and shifting of the teeth caused by tightening of the facial skin can all contribute to joint pain. Bruxism, which refers to involuntary grinding as well as clenching of the teeth, is a common cause of TMJ discomfort. In addition, when the teeth no longer fit together properly, this can increase the strain on the joint. Pain in the jaw and facial muscles can be especially bothersome, since this area is constantly engaged in eating, speaking, swallowing, and even smiling. In some cases, people report sharp, intense, and brief nerve pain. This usually involves the trigeminal nerve, which has several branches across the face, and generally affects only one side of the face. These neuralgic pains can be triggered by chewing or even by a light touch on certain areas of the face. Bone resorption, referring to damage affecting the bone, has been observed at the attachment points of the jaw muscles, particularly at the posterior angle of the lower jaw and in the region of the condyles, located near the ears. These bone changes are usually asymptomatic and are often discovered incidentally during X-rays. |
STRATEGIES FOR IMPROVEMENT
The dentist may carry out selective grinding of misaligned teeth to restore balanced contact and reduce tension or sensitivity. Night guards, also known as occlusal splints, are often worn at night to relieve TMJ pain and protect the teeth from wear. In some cases, anti-inflammatory medication or muscle relaxants may be recommended.
It is advisable to avoid chewing gum and to limit hard or sticky foods to reduce strain on this already sensitive joint. Taking small bites and avoiding always chewing on the same side are also good habits to adopt. Applying warm, moist compresses to painful areas may also help relieve discomfort, especially during more intense episodes.
In cases of trigeminal neuralgia or bone resorption, which are more complex and less common situations, the dentist may recommend a consultation in oral medicine.
Christine Brunet, D.M.D. – Retired Dentist
Christine Brunet is a retired dentist who contributed her clinical expertise to the development of this educational sheet.