Systemic Scleroderma and Cancer
Cancer affects about two in five Canadians over the course of their lives (1). Some individuals diagnosed with systemic scleroderma may also face a concomitant cancer diagnosis. This article discusses the association between scleroderma and cancer, as well as issues and precautions related to the treatment of scleroderma and cancer.
IS THERE AN ASSOCIATION BETWEEN SCLERODERMA AND CANCER?
Individuals with systemic scleroderma have a higher risk of cancer than the general population, particularly within the three to five years surrounding the scleroderma diagnosis. Research studies suggest that scleroderma may be a cross-reactive immune response that arises in the context of an anti-cancer response in certain individuals (2). In other words, the immune system detects cancer cells, tries to fight them by producing antibodies, but also develops antibodies that recognize the body’s normal cells (autoantibodies), leading to the development of scleroderma. When scleroderma develops simultaneously with cancer, it is referred to as “paraneoplastic scleroderma.”
WHO IS AT RISK OF CANCER AROUND THE TIME OF A SCLERODERMA DIAGNOSIS?
The identified risk factors for paraneoplastic scleroderma are the presence of anti-RNA polymerase III and anti-U11/U12-RNP autoantibodies in the blood, as well as older age at the time of diagnosis. Anti-topoisomerase I (or anti-Scl70) autoantibodies may also be associated with a higher risk of paraneoplastic scleroderma, especially in older individuals. Traditional risk factors for cancer development, such as smoking, a strong family history of cancer, or significant unexplained weight loss, are additional elements that should raise suspicion of cancer (2).
IS THERE ALSO A RISK OF CANCER LATER IN THE COURSE OF SCLERODERMA?
Certain manifestations of scleroderma and some medications used to treat scleroderma may also increase the risk of cancer later in the disease. For example, lung fibrosis can increase the risk of developing lung cancer after several years. Chronic irritation of the esophagus due to uncontrolled reflux may also increase the risk of esophageal cancer. Individuals with a concomitant autoimmune liver or thyroid disease may also be at higher risk for cancer affecting these organs. Finally, cyclophosphamide, an immunosuppressive drug used in severe forms of scleroderma, may increase the risk of bladder cancer and hematological cancers, particularly in smokers (2).
WHAT TYPES OF CANCER ARE MOST ASSOCIATED WITH SCLERODERMA?
Individuals with scleroderma have a higher risk of lung, liver, esophageal, and blood cancers (multiple myeloma, leukemia, and lymphoma). Breast cancer is also associated with scleroderma, particularly in the year preceding or following the onset of scleroderma (2, 3).
SHOULD I UNDERGO TESTS FOR CANCER SCREENING?
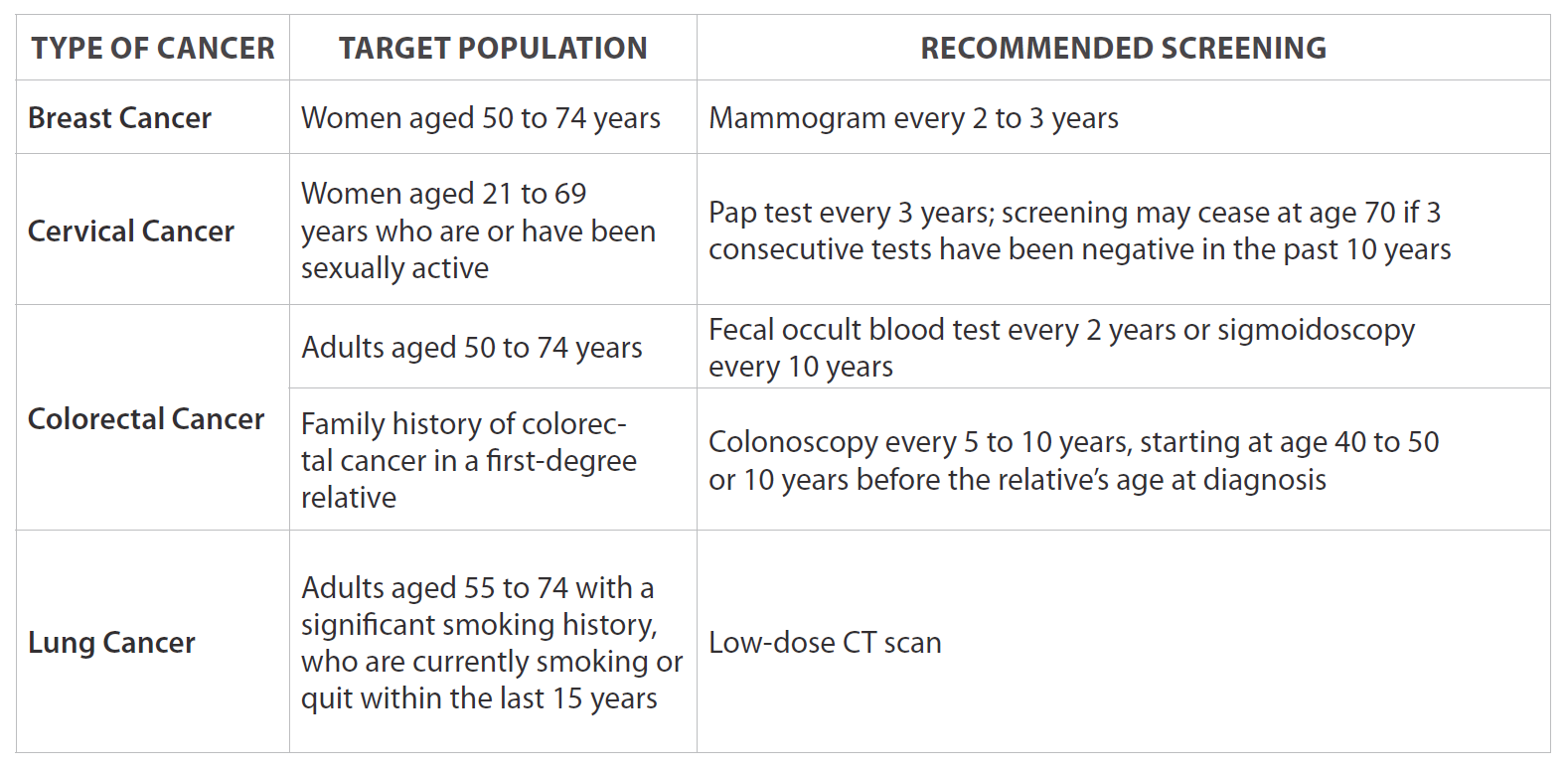
All individuals with scleroderma should undergo cancer screening tests recommended for the general population based on age, sex, and other risk factors (see Table 1) (4), along with a thorough physical examination by their doctor. It is important to note that screening programs vary by province and evolve over time based on available scientific evidence.
For individuals with a recent diagnosis of scleroderma and the risk factors for paraneoplastic scleroderma mentioned above, additional investigations may be considered. Some experts suggest, for instance, annual mammograms, an abdominal-pelvic ultrasound or CT scan, or even a positron emission tomography (PET) scan. However, the optimal screening approach remains to be determined, as few studies currently guide screening practice in patients at higher risk for paraneoplastic scleroderma (2).
Finally, for individuals who have been treated with cyclophosphamide as an immunosuppressive therapy for severe manifestations of scleroderma, annual tests for blood and cancer cells in the urine are recommended to screen for bladder cancer (2).
TABLE 1
CAN RADIATION THERAPY BE USED IN THE CONTEXT OF SCLERODERMA?
One of the possible side effects of radiation therapy is an exaggerated fibrotic reaction at the site of radiation, including the skin (leading to localized scleroderma or morphea) or the lungs (leading to localized pulmonary fibrosis). For this reason, there is concern that radiation therapy could also worsen skin and lung fibrosis in individuals with systemic scleroderma. Systemic scleroderma is therefore generally considered a relative contraindication to radiation therapy. In fact, a few cases have been reported in the literature of the onset or worsening of skin or lung fibrosis in individuals with scleroderma who received radiation therapy, particularly in the context of breast cancer.
However, in a large recent study reporting the experience of nearly 70 women with systemic scleroderma who received radiation therapy for breast cancer, exaggerated local skin fibrosis in the irradiated breast area was observed in half of the patients, and localized lung fibrosis at the irradiation site was observed in only 10% of patients (5). Moreover, no worsening of systemic scleroderma skin or lung involvement was observed.
Thus, radiation therapy is a therapeutic option that may be considered in individuals with systemic scleroderma but should be discussed, weighing the expected benefits on cancer against the potential associated risks.
IS CHEMOTHERAPY SAFE IN THE CONTEXT OF SCLERODERMA?
Chemotherapy is often the basis of cancer treatments, and the vast majority of these treatments are safe in the context of scleroderma. However, certain chemotherapies, notably taxanes (docetaxel, paclitaxel) and gemcitabine, are known to have the rare (<1%) side effect of inducing skin hardening similar to limited or diffuse scleroderma, and sometimes even severe Raynaud’s phenomenon. Bleomycin can also induce pulmonary fibrosis and, more rarely, skin fibrosis (6, 7).
However, the safety of these drugs has not been specifically studied in individuals with systemic scleroderma. Nevertheless, given the rare but well-documented risks of drug-induced scleroderma, it is important that oncologists and rheumatologists discuss the risks, benefits, and treatment alternatives with the patient when such chemotherapy is being considered.
CAN IMMUNE CHECKPOINT INHIBITORS BE USED IN THE CONTEXT OF SCLERODERMA?
Immune checkpoint inhibitors (such as nivolumab, pembrolizumab, and durvalumab) are drugs that help the patient’s own immune system to fight their cancer. These drugs have revolutionized the treatment of certain otherwise incurable cancers. However, in some patients, these drugs can overstimulate the immune system, leading to the onset of new autoimmune diseases, including scleroderma (<1%).
The safety of these drugs in individuals with systemic scleroderma was studied in 17 patients: 4 (24%) of them experienced a severe flare of their disease. The risk may be higher in patients with diffuse scleroderma (flare in 3/9) than in those with limited scleroderma (flare in 1/9), and particularly in those with the anti-RNA polymerase III autoantibody (flare in 2/2) (8).
Ultimately, the risks and benefits of treatment with an immune checkpoint inhibitor must be discussed with the patient in close collaboration with their oncologist and rheumatologist.
CONCLUSION
In summary, individuals living with scleroderma are at a higher risk of developing cancer compared to the general population. Cancer screening is recommended and should be personalized based on age, sex, and risk factors. Radiation therapy, chemotherapy, and immune checkpoint inhibitors are therapeutic options that can be considered. Close collaboration between the rheumatologist, oncologist, and patient is necessary to discuss the risks, benefits, and treatment alternatives, in order to minimize the risks of exacerbating the autoimmune disease while maximizing the chances of curing the cancer.
REFERENCES:
1. Canadian Cancer Statistics Advisory Committee, in collaboration with the Canadian Cancer Society, Statistics Canada, and the Public Health Agency of Canada. Toronto (Ontario) Canadian Cancer Society; 2023 [Available from: cancer.ca/Canadian-Cancer-Statistics-2023-FR].
2. Weeding E, Casciola-Rosen L, Shah AA. Cancer and Scleroderma. Rheum Dis Clin North Am. 2020;46(3):551-64.
3. Bonifazi M, Tramacere I, Pomponio G, Gabrielli B, Avvedimento EV, La Vecchia C, et al. Systemic sclerosis (scleroderma) and cancer risk: systematic review and meta-analysis of observational studies. Rheumatology (Oxford). 2013;52(1):143-54.
4. Chaput G, Del Giudice ME, Kucharski E. Cancer screening in Canada: What’s in, what’s out, what’s coming. Can Fam Physician. 2021;67(1):27-9.
5. Shah DJ, Hirpara R, Poelman CL, Woods A, Hummers LK, Wigley FM, et al. Impact of Radiation Therapy on Scleroderma and Cancer Outcomes in Scleroderma Patients With Breast Cancer. Arthritis Care Res (Hoboken). 2018;70(10):1517-24.
6. Ketpueak T, Chanloung W, Nan KN, Pongsananurak C, Kasitanon N, Louthrenoo W. Paclitaxel-induced diffuse scleroderma with possible scleroderma-renal crisis: a case report and literature review of taxanes-induced scleroderma. Clin Rheumatol. 2022;41(12):3887-96.
7. Cappelli LC, Shah AA. The relationships between cancer and autoimmune rheumatic diseases. Best Pract Res Clin Rheumatol. 2020;34(1):101472.
8. Panhaleux M, Espitia O, Terrier B, Manson G, Maria A, Humbert S, et al. Anti-programmed death ligand 1 immunotherapies in cancer patients with pre-existing systemic sclerosis: A postmarketed phase IV safety assessment study. Eur J Cancer. 2022;160:134-9.
November 2024