Capillaroscopy & Complementary Observations
Nailfold capillaroscopy is a simple, non-invasive, painless examination mainly performed on the hands that allows the study of small blood vessels, called capillaries, located around the nail beds. After depositing a drop of oil to make the skin more transparent, the periungual capillaries are observed under a microscope. The observation of animal and human cells began more than 300 years ago, and the addition of a magnifying glass 100 years later allowed the observation of capillaries at the surface of the skin. Over 100 years ago, significant changes in capillary morphology have been observed during scleroderma; and, in the last 40 years, studies have been carried out showing the morphological evolution of capillaries in relation to scleroderma-specific antibodies.
THE FUNCTIONS OF THE CAPILLARIES
The capillaries, so named for their resemblance to hair, although they are ten times smaller, are the smallest visible vascular structure on the skin. They form a loop that connects the smallest end of the arteries to that of the veins. They act as a barrier that filters certain structures, bringing essential nutrients to the surrounding cells and capturing waste products that are then eliminated by other organs. With today’s high-magnification microscopes (from 50 to 200 times) their shapes can be accurately revealed thanks to the red blood cells that circulate in them and which define their contours since their walls, made up of just a few cells, are too thin to be visible.
WHY PERFORM A CAPILLAROSCOPY?
Diagnostic criteria for scleroderma have gradually evolved, as these were initially based on the degree of skin and lung involvement (1980). Later, the growing interest of clinicians and researchers in this disease, the introduction of capillaroscopy, the notion of Raynaud’s phenomenon and the discovery of scleroderma-specific antibodies have led to the development of new diagnostic criteria (1988, 2001). Since 2013, following a consensus between American and European physicians on what are the key features for diagnosing scleroderma, new diagnostic criteria are being used. These criteria are based on a points-scoring system that relies on the presence of certain physical aspects (cutaneous and pulmonary), Raynaud’s phenomenon, capillary abnormalities and specific antibodies found in 85% of cases (anticentromere (ACA), anti-topoisomerase, anti-Th, anti-RNA Polymerase 3).
CAPILLARY CHANGES IN SCLERODERMA
The presence of specific abnormalities of the nailfold capillaries provides further evidence for supporting the diagnosis of scleroderma especially in the absence of specific antibodies (15% of cases). An examination is required when a patient develops symptoms in the hands, whether or not these are related to Raynaud’s phenomenon. Capillary abnormalities are not necessarily related to the number of fingers affected or the frequency of episodes of capillary discoloration.
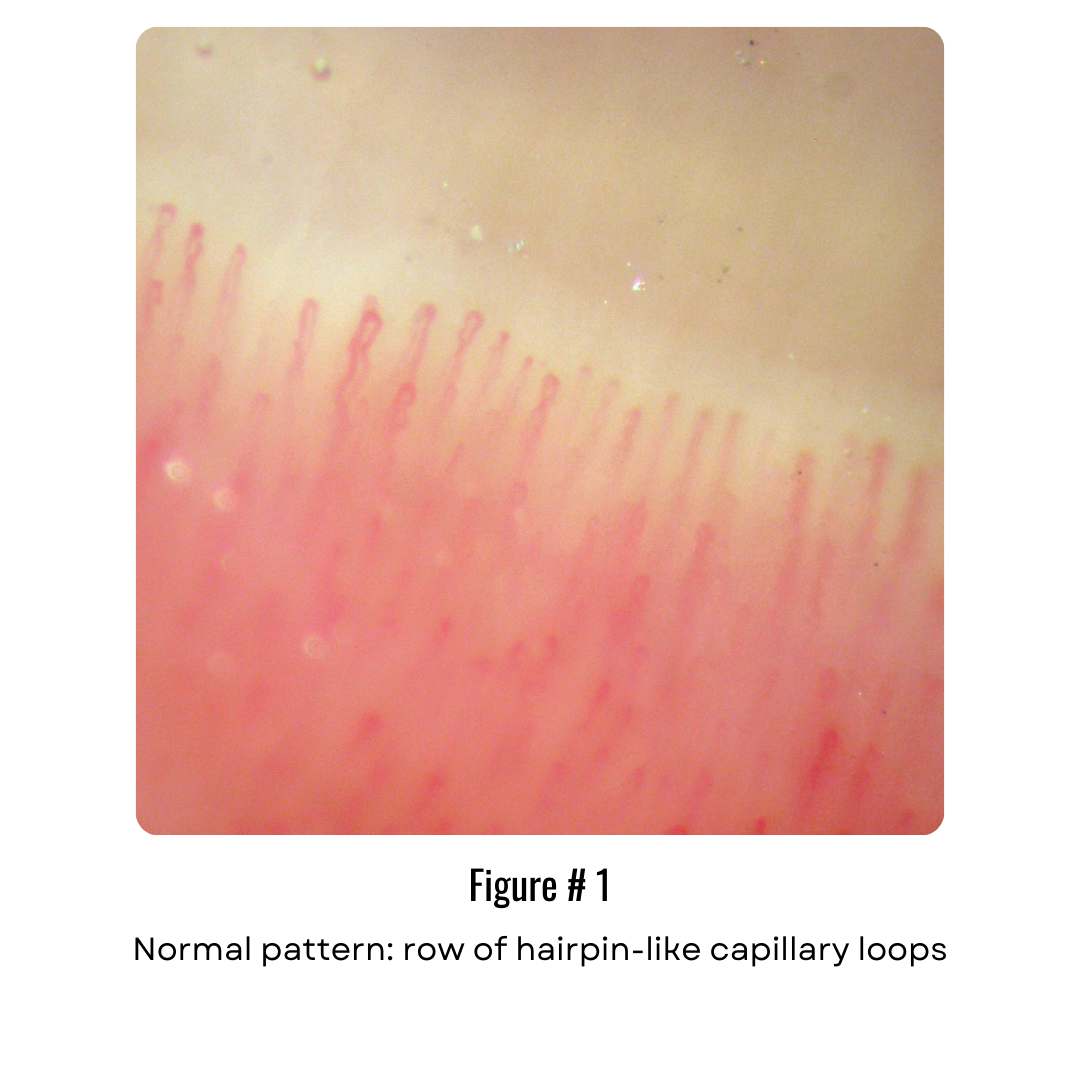
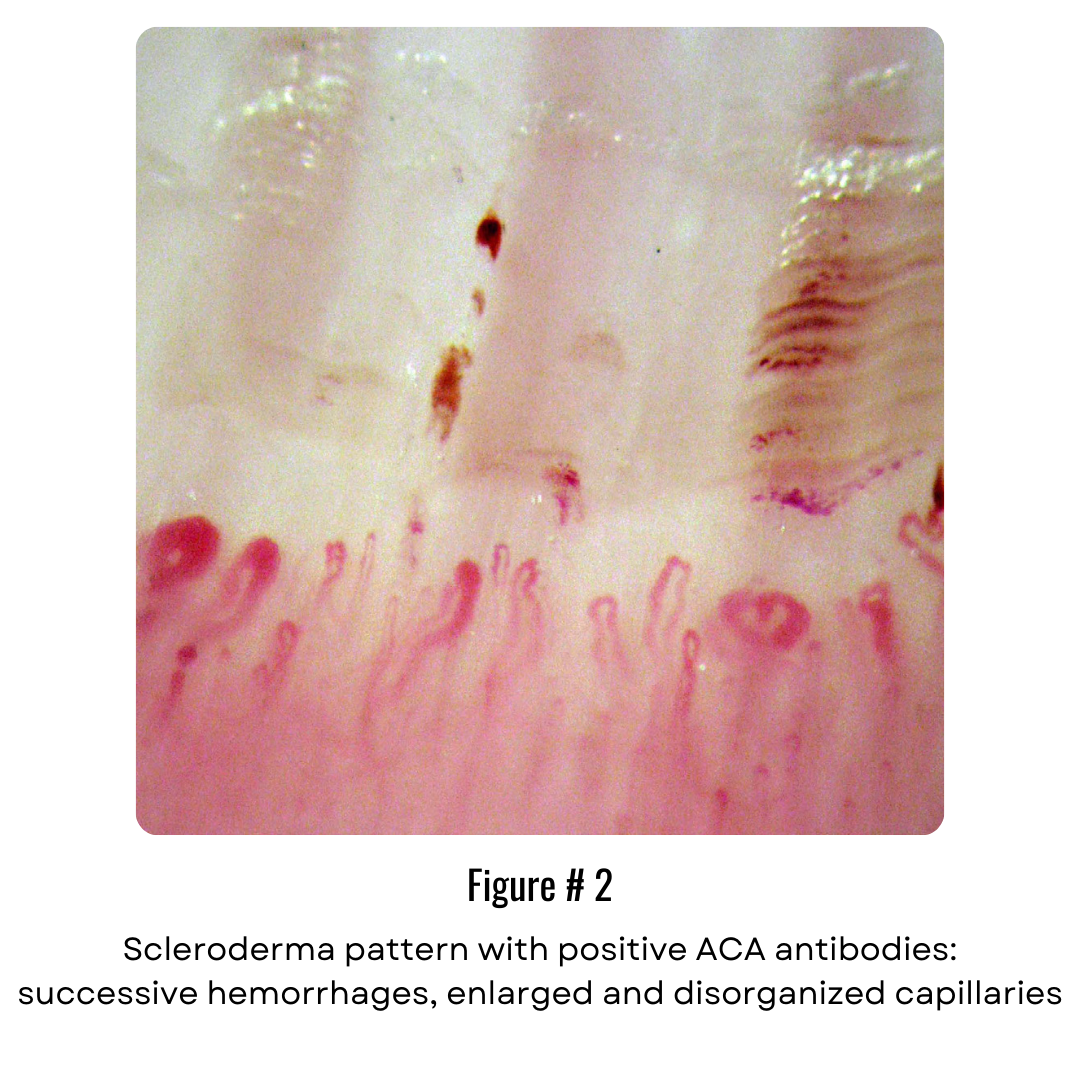
In scleroderma, the walls of the capillaries and the surrounding tissue appear to change more or less rapidly depending on the antibodies detected and disease duration: normal pattern appears as a row of hairpin-like capillary loops (figure # 1) become disorganized. The capillary loops enlarge, at more than 50 μm (figure # 2), they thrombosed (self-destruct) and disappear with or without a trace of bleeding. They may cluster together and are often visible as small red dots on the skin surface (capillary telangiectasias) with little evidence of replacement of the missing vessels (angiogenesis). Changes in capillaries have been observed up to 15 years before the onset of skin or other internal organs involvement during scleroderma. However, some patients with long-standing scleroderma may have normal capillaries.
Nailfold capillaroscopy alone does not allow for the diagnosis of scleroderma in all cases because the capillaries may also be enlarged in patients with other autoimmune diseases such as lupus erythematosus and dermatomyositis. Capillaroscopy findings should thus be interpreted according to some specific questions, the clinical examination and the antibodies detected.
Capillaroscopy remains an important tool for the early diagnosis of scleroderma. The pathophysiological mechanisms leading to changes in the number of capillaries, their shape and arrangement during the course of the disease are still poorly understood, as is the relationship with the antibodies detected. Fortunately, research continues to provide a better understanding of this disease and to identify treatments that are not only curative but also preventive.